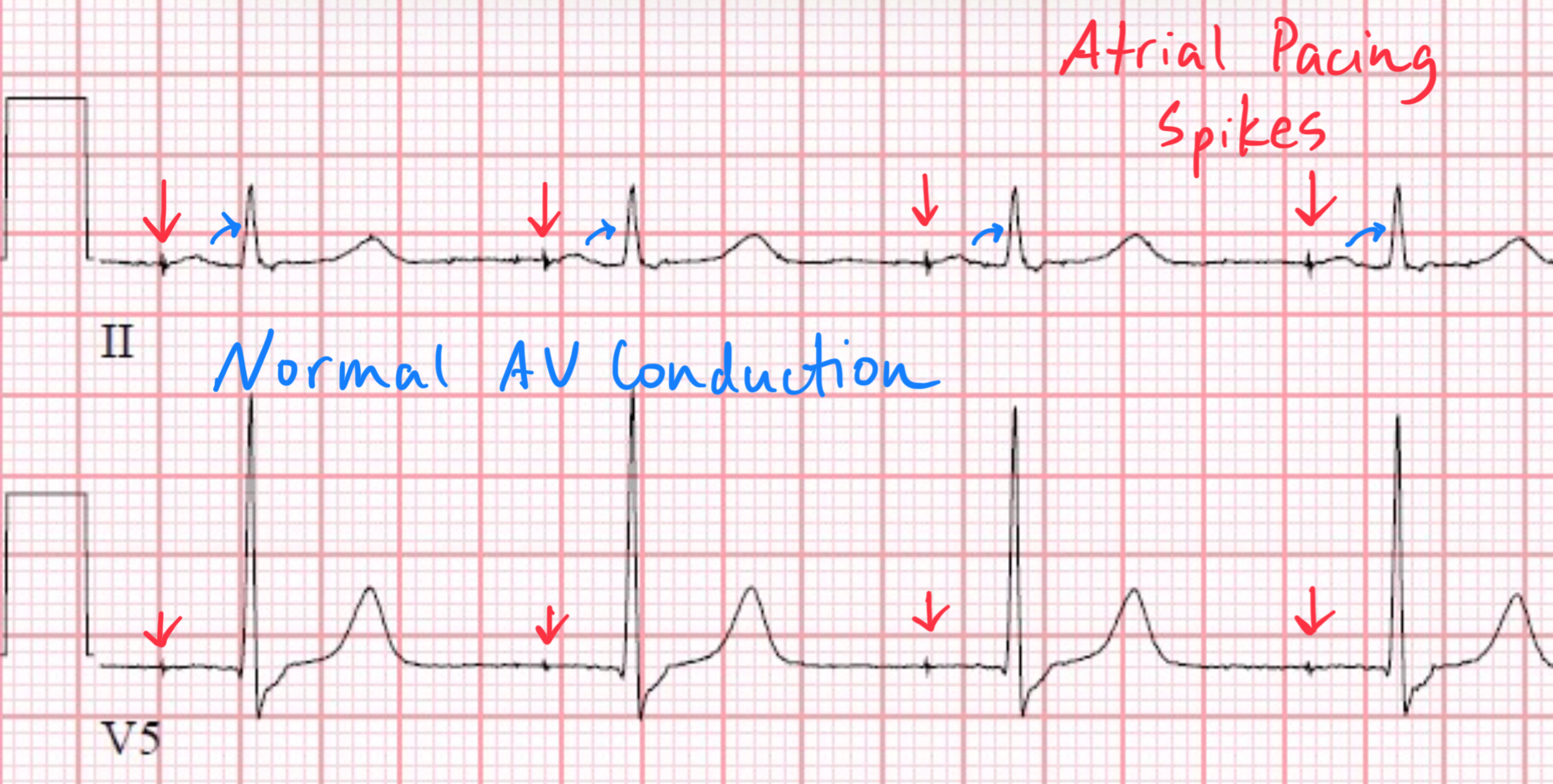
Atrial-Paced, Ventricular-Sensed Rhythms
Dec 04, 2025Dual-chamber pacemakers programmed in DDD mode often generate a rhythm where the atrium is paced but the ventricle is allowed to conduct normally and is merely sensed. This pattern—atrial-paced, ventricular-sensed (AP–VS)—is one of the most physiologic expressions of DDD pacing, because it preserves native His–Purkinje ventricular activation while still supporting atrial function when the sinus node cannot.
This post explains why dual-chamber pacemakers behave this way, how the device times atrial pacing and ventricular sensing, and what anatomy makes this pacing strategy possible.
Related Posts:
1. Why Does a Dual-Chamber Pacemaker Pace the Atrium but Sense the Ventricle?
Because many patients with DDD devices have:
-
Sinus node dysfunction
-
Intact AV conduction
-
A normal His–Purkinje system
In these patients, the pacemaker's job is to:
-
Augment or replace sinus node function (atrial pacing)
-
Allow the patient’s intrinsic AV node and His–Purkinje conduction to activate the ventricles normally(ventricular sensing)
-
Avoid unnecessary ventricular pacing, which causes dyssynchronous contraction and higher long-term morbidity
Thus, in an AP–VS rhythm, the pacemaker provides atrial timing support but still trusts (but verifies) the native AV system to conduct the impulse.
2. Timing Cycles That Create an AP–VS Sequence
Dual-chamber timing requires coordination of atrial pacing, atrial sensing, ventricular sensing, and AV delay monitoring. Here is how the pacemaker produces an atrial-paced, ventricular-sensed beat:
Step 1 — Atrial Pace Delivered
When the sinus node fails to fire within the Lower Rate Interval (LRI), the pacemaker emits an atrial pacing spike.
This creates an artificial P wave that behaves as if it originated from the sinus node.
Step 2 — AV Delay Timer Starts
Immediately after the atrial pace, the pacemaker begins the AV delay interval (e.g., 150–200 ms).
This is the key distinction from AAI pacing:
Dual-chamber devices always initiate an AV delay after every atrial event—paced or sensed.
The device now “waits” to see if the ventricle activates on its own.
Step 3 — Ventricular Sensing Window Opens
During the AV delay, the pacemaker monitors for a native ventricular depolarization (VS).
If a normal QRS complex appears in this window, the pacemaker:
-
Marks it as ventricular sensed
-
Inhibits ventricular pacing (VP)
-
Resets timing intervals for the next beat
This produces the AP–VS sequence:
- Atrial Pace → AV Delay → Ventricular Sense
(No ventricular pacing required)
Step 4 — If No Ventricular Sensing Occurs → Ventricular Pace
If the AV delay expires without a sensed QRS, the pacemaker assumes loss of AV conduction and delivers a ventricular pacing spike (VP).
This yields an AP–VP pattern.
Thus:
-
AP–VS = intact AV conduction
-
AP–VP = AV nodal disease or prolonged block
Enjoy ECG Lectures with Reid? Here is a special gift from Reid
100 High Yield Annotated ECGs
Click below to download this free resource.