Why Left Ventricular Hypertrophy Can Cause Secondary QRS Widening on the ECG
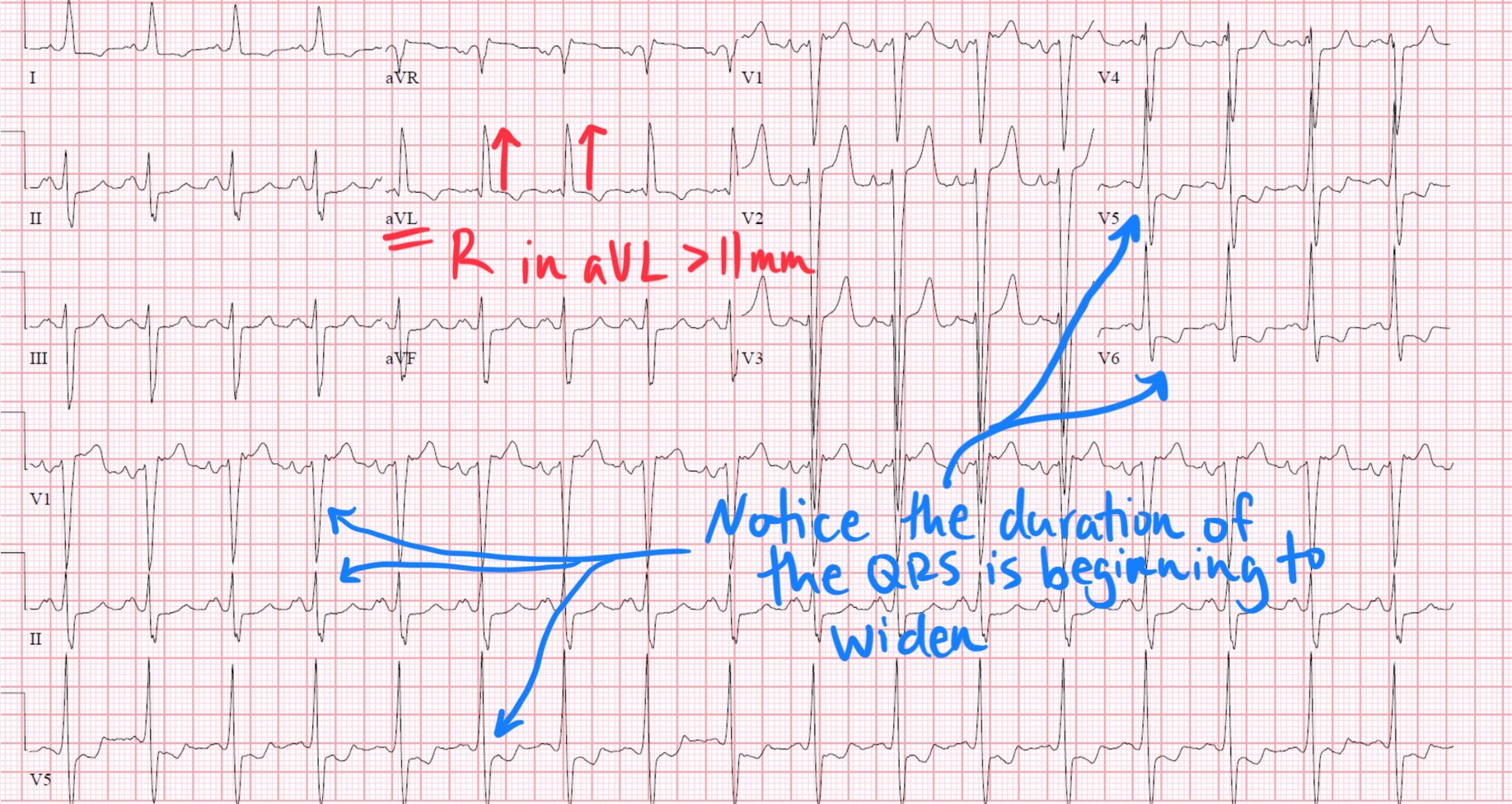
Jun 07, 2025Left ventricular hypertrophy (LVH) is most often recognized on ECG by increased QRS voltage—tall R waves in left-sided leads and deep S waves in right-sided leads. However, in some cases, LVH is also associated with a widened QRS complex, raising the question: Why would a structural enlargement of the left ventricle affect the duration of depolarization?
This article explores the electrophysiological consequences of LVH, focusing on the mechanisms behind QRS widening, and how this represents a form of secondary conduction delay due to myocardial remodeling.
What Defines Left Ventricular Hypertrophy?
LVH is a structural adaptation to chronically increased afterload, most commonly from:
-
Systemic hypertension
-
Aortic stenosis
-
Hypertrophic cardiomyopathy
The left ventricular wall thickens—sometimes concentrically, sometimes asymmetrically—leading to:
-
Increased myocardial mass
-
Disrupted fiber orientation
-
Altered conduction pathways
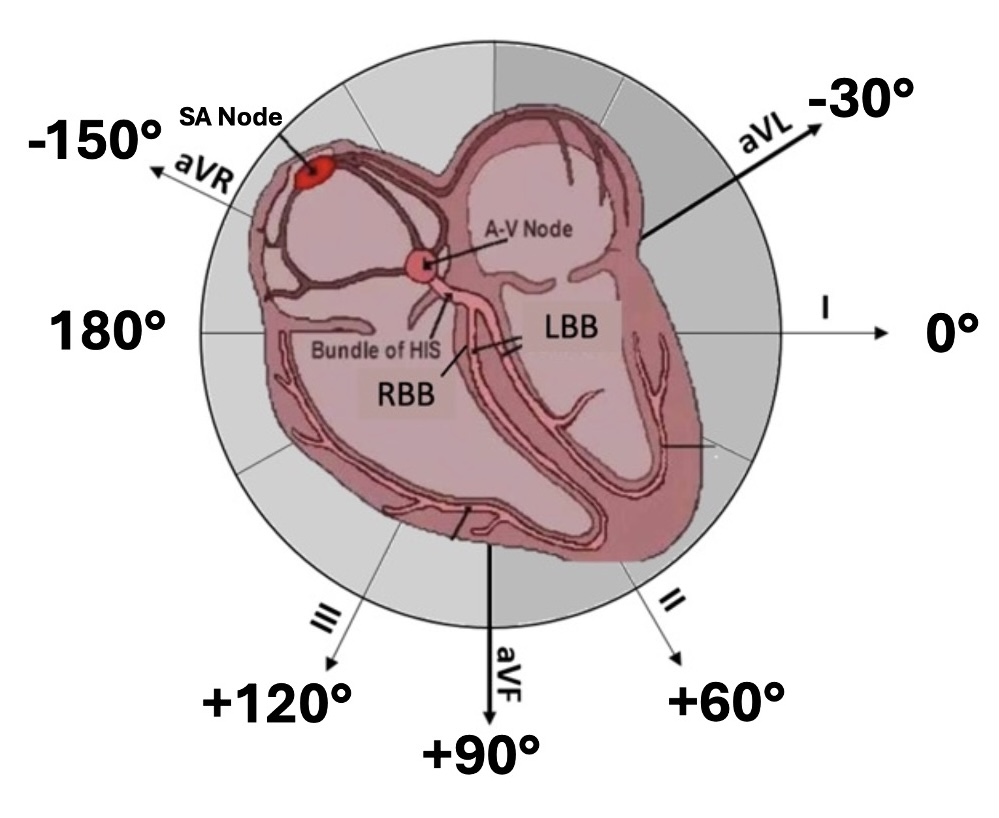
Normal Ventricular Depolarization: A Quick Review
Under normal conditions:
-
The His-Purkinje system ensures rapid and synchronous depolarization of both ventricles.
-
Left and right bundle branches deliver impulses nearly simultaneously, resulting in a narrow QRS complex (< 100 ms).
The QRS width reflects the speed and coordination of ventricular depolarization, not just the size of the ventricles.
Mechanisms Behind QRS Widening in LVH
Although bundle branch blocks (such as left bundle branch block) are classic causes of QRS widening, LVH can also result in secondary QRS prolongation through the following mechanisms:
1. Increased Myocardial Mass = Increased Conduction Distance
-
The hypertrophied left ventricle is physically larger.
-
Electrical impulses must travel a greater distance to activate all myocytes.
-
Even with intact conduction pathways, this increased conduction length leads to longer depolarization time and a broader QRS.
2. Disrupted Myocardial Architecture
-
Hypertrophied myocardium develops fibrosis, disorganized fibers, and heterogeneous conduction properties.
-
This leads to slower intramyocardial conduction, especially in lateral and posterior walls, prolonging the terminal portion of the QRS.
3. Relative Delay in Left Ventricular Activation
-
Although not a classic bundle branch block, LVH can cause asynchronous ventricular activation.
-
The hypertrophied lateral wall may depolarize later than the septum or apex.
-
This is sometimes referred to as a "strain pattern" and can contribute to QRS widening and terminal QRS notching.
4. Subclinical Conduction System Disease
-
Many patients with LVH, especially from longstanding hypertension, may also have fibrosis in the left bundle branch system, resulting in incomplete conduction delays that don’t meet full LBBB criteria but still widen the QRS.
ECG Clues: When QRS Widening Is Due to LVH
Look for:
-
QRS duration > 100 ms, but not necessarily > 120 ms (which would suggest bundle branch block)
-
Classic voltage criteria for LVH:
-
S wave in V1 + R wave in V5 or V6 ≥ 35 mm
-
R wave in aVL ≥ 11 mm
-
-
Left axis deviation
-
Prolonged intrinsicoid deflection in left-sided leads (time from QRS onset to R wave peak)
-
Secondary ST-T changes (strain pattern) in lateral leads
Distinguishing LVH-Related QRS Widening from Bundle Branch Block
| Feature | LVH with Widened QRS | LBBB or RBBB |
|---|---|---|
| QRS duration | Mildly prolonged (100–120 ms) | Markedly prolonged (>120 ms) |
| Depolarization sequence | Preserved but slowed | Altered activation pattern |
| QRS morphology | Normal axis, strain patterns | Specific BBB morphology (RSR’, wide notches) |
| Cause | Myocardial thickening/fibrosis | Conduction system block |
Clinical Relevance
QRS widening in LVH is not always benign. It often reflects:
-
More advanced structural remodeling
-
Subclinical conduction disease
-
Higher risk of arrhythmias and heart failure
It may also affect interpretation of other ECG features:
-
ST depression and T wave inversion may be mistaken for ischemia
-
QRS widening may obscure subtle bundle branch blocks or fascicular blocks
Summary: Why LVH May Cause QRS Widening
| Mechanism | Effect on QRS |
|---|---|
| Increased myocardial mass | Longer conduction path, prolonged QRS |
| Fibrosis and architectural disarray | Slowed conduction, delayed terminal QRS |
| Delayed activation of hypertrophied regions | Broader, sometimes notched QRS |
| Subclinical conduction system involvement | Incomplete or diffuse conduction delay |
Clinical Takeaway
While voltage is the hallmark of LVH on ECG, QRS widening may be an underappreciated consequence. It reflects not just the size of the myocardium, but the integrity of conduction pathways, the presence of fibrosis, and the synchrony of activation. Recognizing this pattern helps refine your interpretation of complex ECGs and may point toward more significant underlying cardiac disease.
Enjoy 'The ECG Blog with Reid'?