The Anatomy of Pathological Q Waves on ECG
Jun 03, 2025Pathological Q waves are among the most recognizable signs of a prior myocardial infarction (MI) on the electrocardiogram. Yet their presence is not always straightforward. To understand their significance, we need to explore the electrophysiological mechanisms and cardiac anatomy that give rise to these uniquely informative deflections.
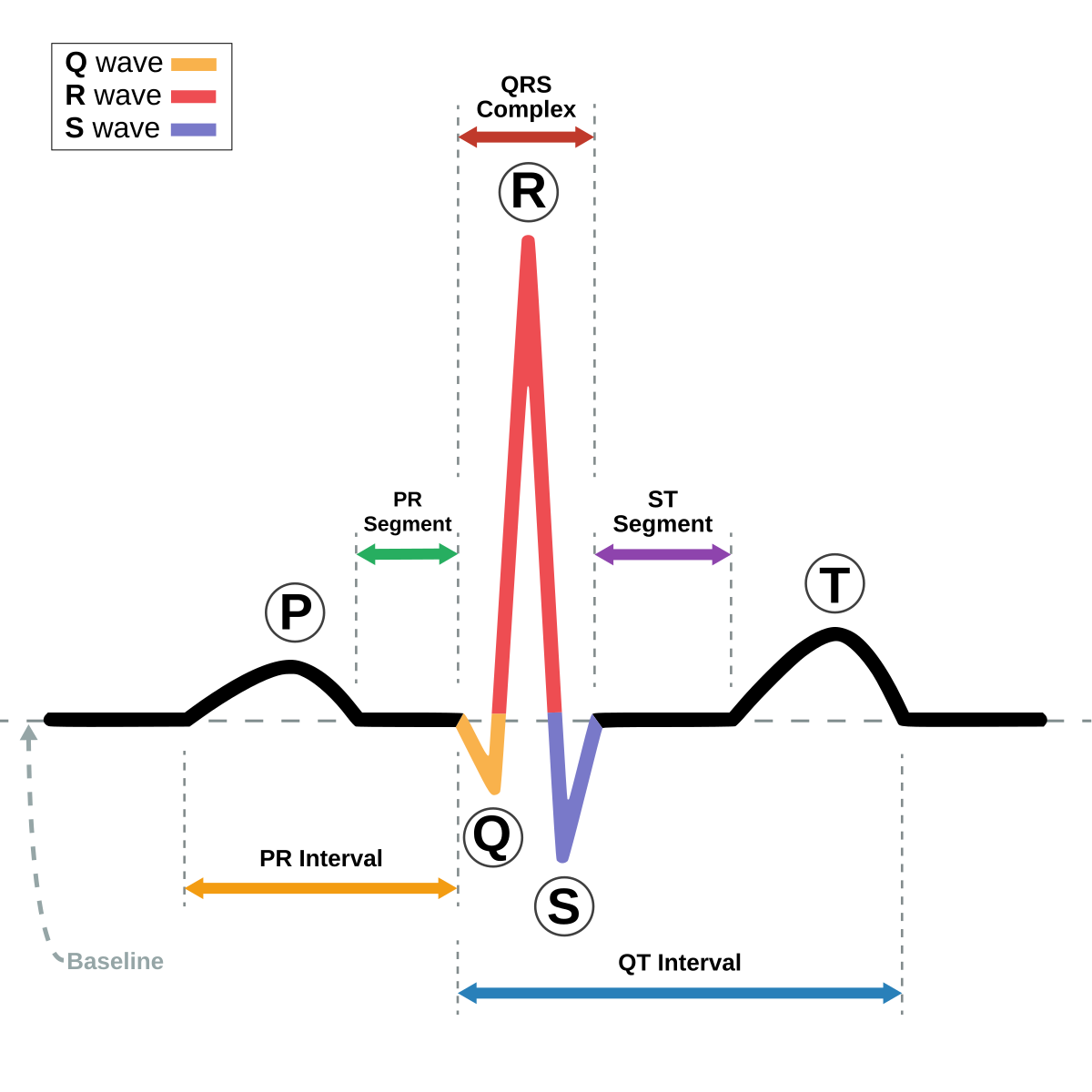
What Is a Q Wave?
A Q wave is the first negative deflection of the QRS complex—appearing before any upward deflection (R wave). It represents the initial vector of ventricular depolarization as seen from a particular lead.
https://en.wikipedia.org/wiki/QRS_complex
Not all Q waves are abnormal. Small, narrow Q waves may be seen in several leads as a part of normal physiology. However, when Q waves are wide, deep, or in unexpected locations, they may be pathological, indicating the presence of non-viable, infarcted myocardium.
When Is a Q Wave Pathological?
A Q wave becomes pathological when it reflects electrically silent tissue, usually due to transmural myocardial infarction. The commonly accepted criteria for pathological Q waves are:
-
Duration ≥ 0.04 seconds (one small box)
-
Depth ≥ 25% of the amplitude of the succeeding R wave, or > 2 mm deep in at least two contiguous leads
-
Presence in contiguous leads that represent a specific myocardial territory
These criteria help differentiate infarction-related Q waves from benign variants seen in normal individuals.
The Anatomy Behind Pathological Q Waves
To understand the Q wave’s significance, consider what happens during normal ventricular depolarization versus what occurs during or after a transmural infarct.
In Normal Physiology
-
Depolarization spreads across the ventricles in an organized, endocardium-to-epicardium pattern.
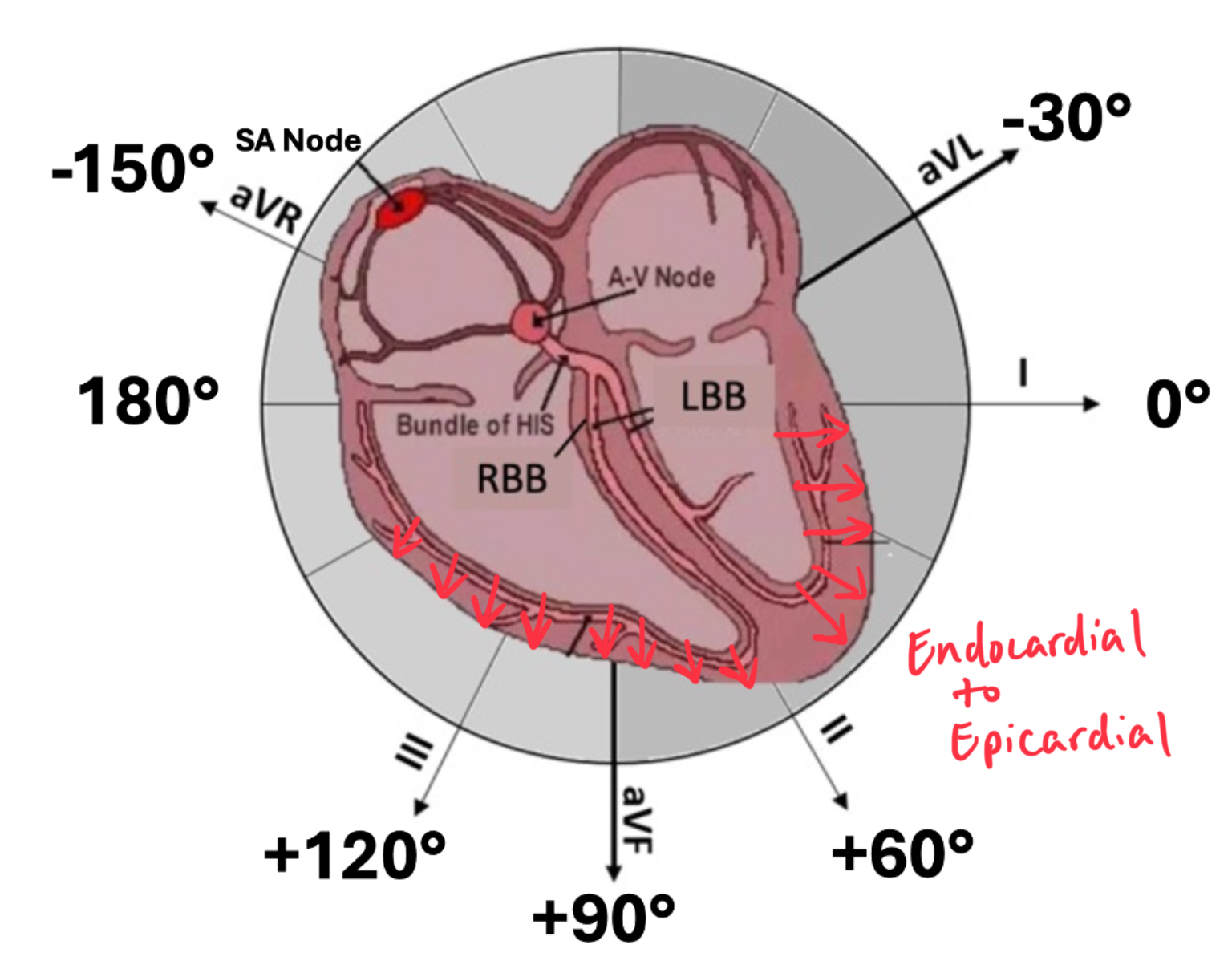
-
All regions contribute to the generation of electrical vectors recorded on the ECG.
In Infarcted Myocardium
-
Transmural infarction results in a full-thickness area of myocardium that becomes electrically inert.
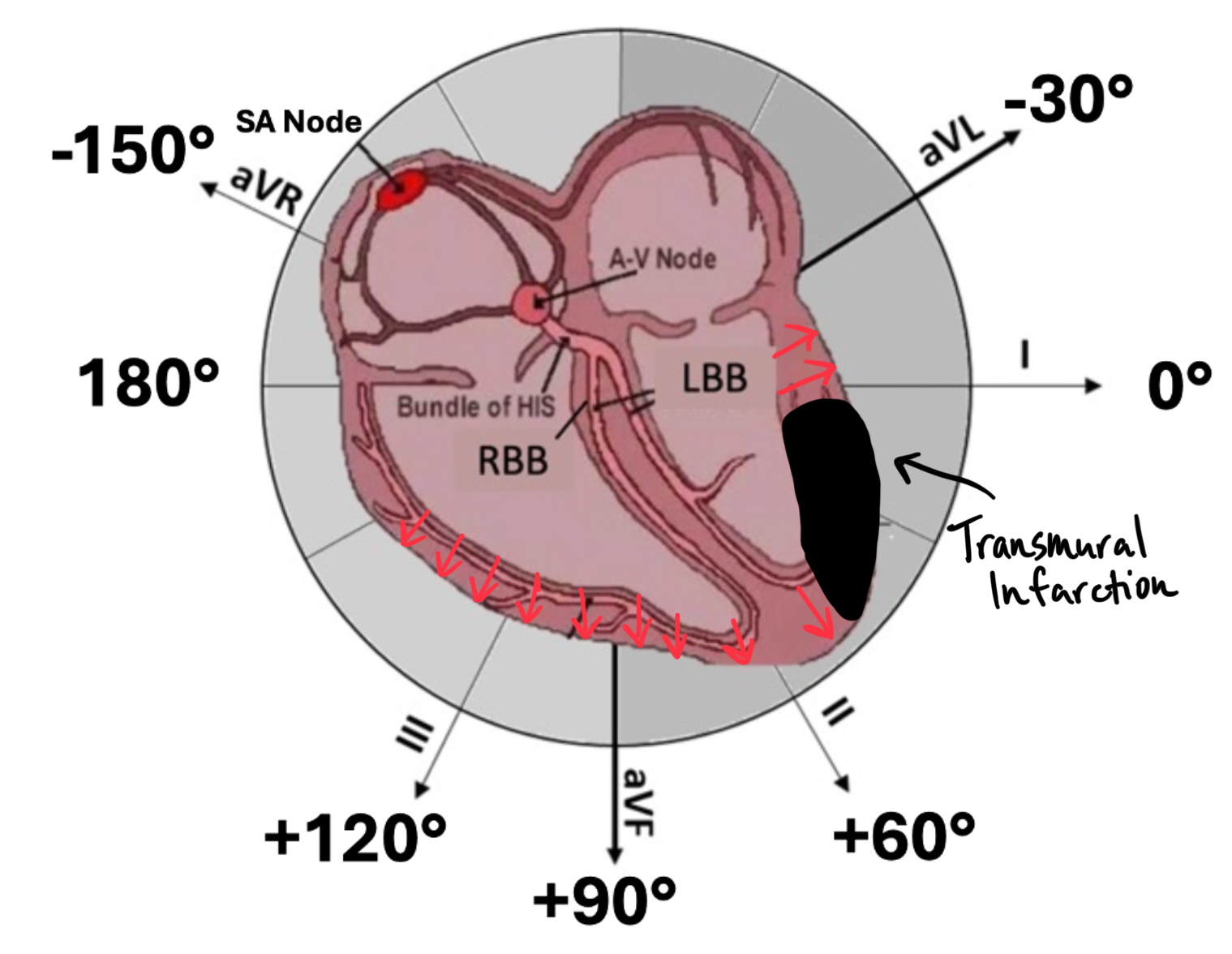
-
This region no longer participates in depolarization.
-
The absence of opposing electrical activity from the infarcted area causes the initial vector of depolarization to shift away from the infarcted tissue.
-
If the ECG lead is positioned over this infarcted zone, it records a negative deflection—a pathological Q wave—at the start of the QRS complex.
Importantly, this negative deflection does not represent active depolarization of the infarcted zone. Instead, it reflects the net direction of surviving myocardial depolarization, now unopposed by the damaged region.
Regional Patterns of Pathological Q Waves
The location of the Q wave provides information about the territory of infarction and, by extension, the affected coronary artery.
| MI Territory | Leads with Q Waves | Likely Artery Involved |
|---|---|---|
| Anterior MI | V1–V4 (V1-2 Septal) | Left Anterior Descending (LAD) |
| Inferior MI | II, III, aVF | Right Coronary or LCx |
| Lateral MI | I, aVL, V5–V6 | Left Circumflex (LCx) |
| Posterior MI* | Tall R in V1–V2 (reciprocal Q) | RCA or LCx |
*Posterior infarctions do not produce direct Q waves but may present as tall R waves in V1–V2, the mirror image of a Q wave seen from the posterior wall.
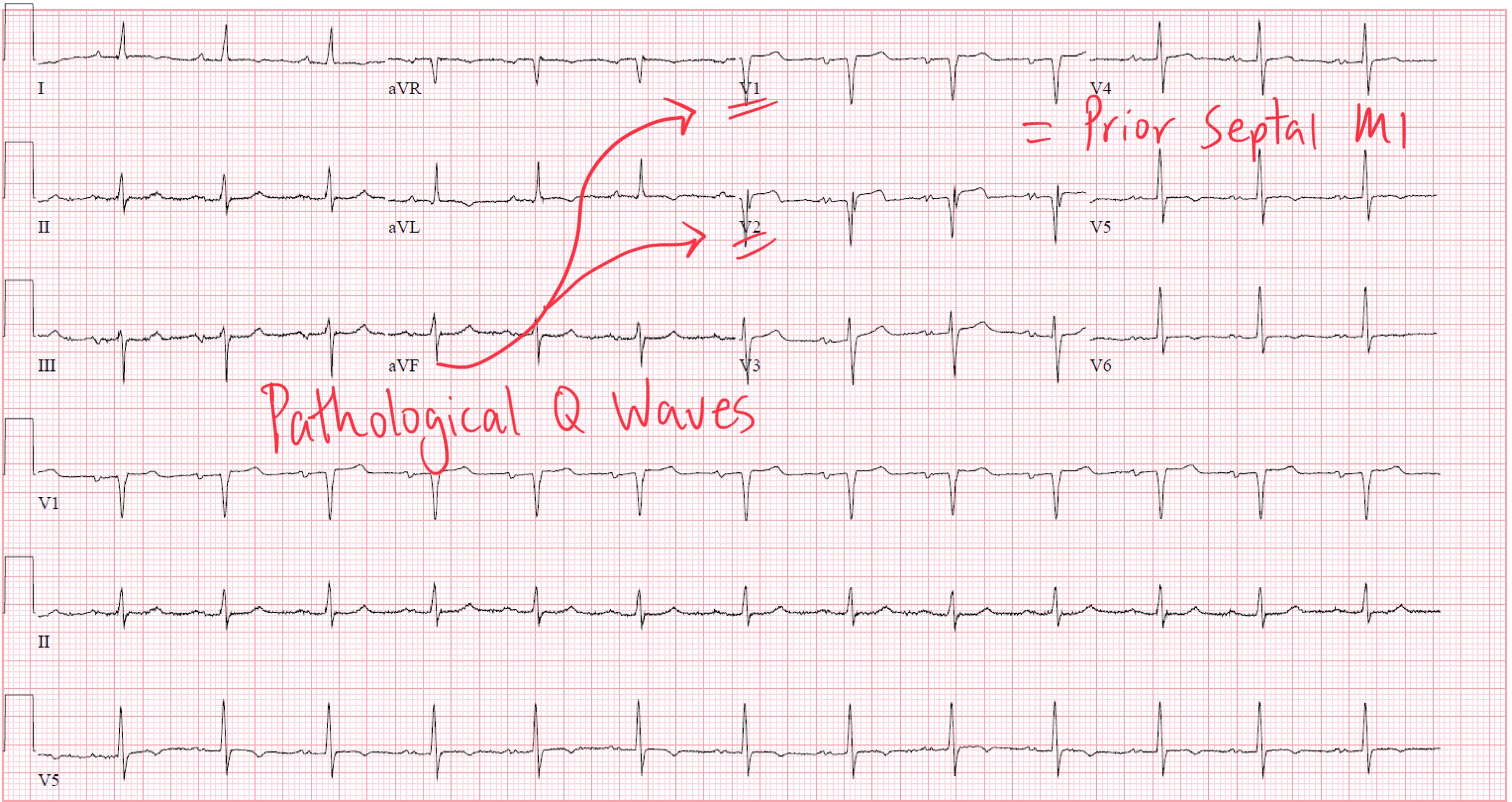
Prior Septal MI
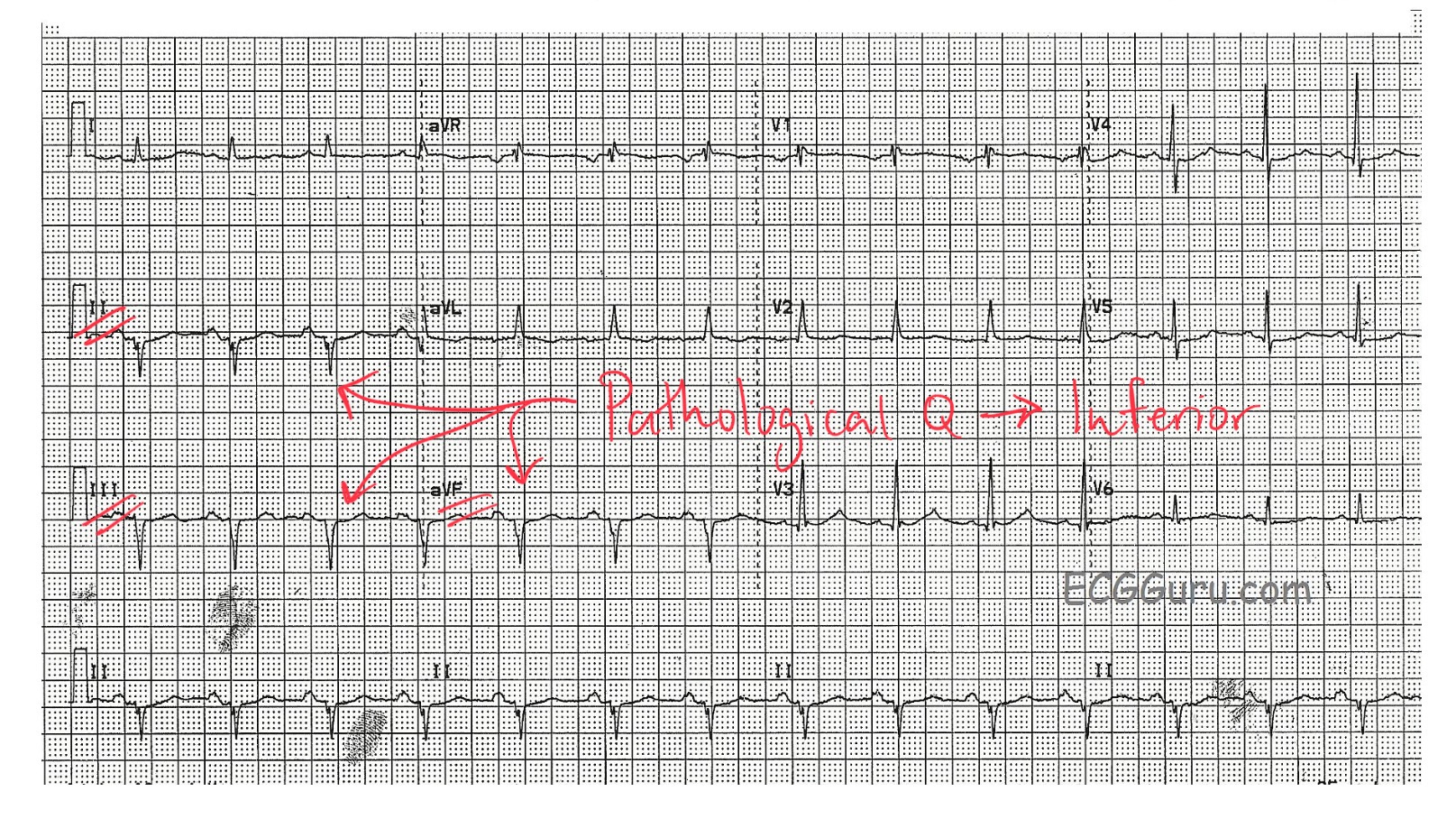
Prior Inferior MI (from my friends at ECGGuru.com)
Q Waves Can Be Reversible
Though often considered a permanent marker of infarction, pathological Q waves may regress over time. Factors influencing reversibility include:
-
Timely reperfusion therapy
-
Subendocardial rather than full-thickness injury
-
Recovery from stunned or hibernating myocardium
Therefore, while Q waves suggest past infarction, their absence does not always rule one out, and their presence may evolve with time.
Mimics and Misinterpretation: When Q Isn’t Q
Several conditions may mimic pathological Q waves:
-
Normal septal Q waves (especially in leads I, aVL, V5–V6)
-
Left ventricular hypertrophy (pseudo-infarct pattern)
-
Hypertrophic cardiomyopathy
-
Lead misplacement
-
Infiltrative disease (e.g., amyloidosis)
Clinical correlation is essential. Do not rely on the ECG alone. Always consider the patient’s symptoms, cardiac history, and findings from imaging or biomarkers.
Clinical Takeaway
Pathological Q waves are not active signals—they are silent footprints of a damaged heart wall. Their presence reflects an electrically dead zone of myocardium, where no depolarization occurs, shifting the electrical vectors recorded on surface ECG leads. When interpreted with context, they offer powerful insight into past infarction, infarct location, and extent of myocardial damage.
Enjoy ECG Lectures with Reid? Here is a special gift from Reid
100 High Yield Annotated ECGs
Click below to download this free resource.