The Anatomy Behind the P-Wave Terminal Force in V1
Dec 01, 2025The P-wave terminal force in V1 (PTFV1) is one of the most anatomically honest measurements on the ECG. It is not simply a marker of “left atrial enlargement”—it is the surface reflection of how the atria depolarize in sequence, how their masses compare, and how the interatrial conduction system distributes the sinus impulse. To understand PTFV1, you must start with the anatomy of Bachmann’s bundle.
1. Normal Atrial Activation: A Biphasic Process
Sinus impulses originate high in the right atrium and spread in two broad waves:
A. Right atrial depolarization
-
Occurs first.
-
Directed anteriorly.
-
Produces the initial positive deflection in V1.
B. Left atrial depolarization
-
Occurs second.
-
Requires interatrial conduction through Bachmann’s bundle—the dominant anterior interatrial tract.
-
Produces a vector directed posteriorly and leftward, away from V1.
-
This becomes the terminal negative deflection of the P wave in V1.
The biphasic P wave in V1 is thus the direct sum of:
-
Early RA activation (positive)
-
Later LA activation (negative)
V1 is uniquely positioned (right parasternal, anterior) to show this sequence clearly.
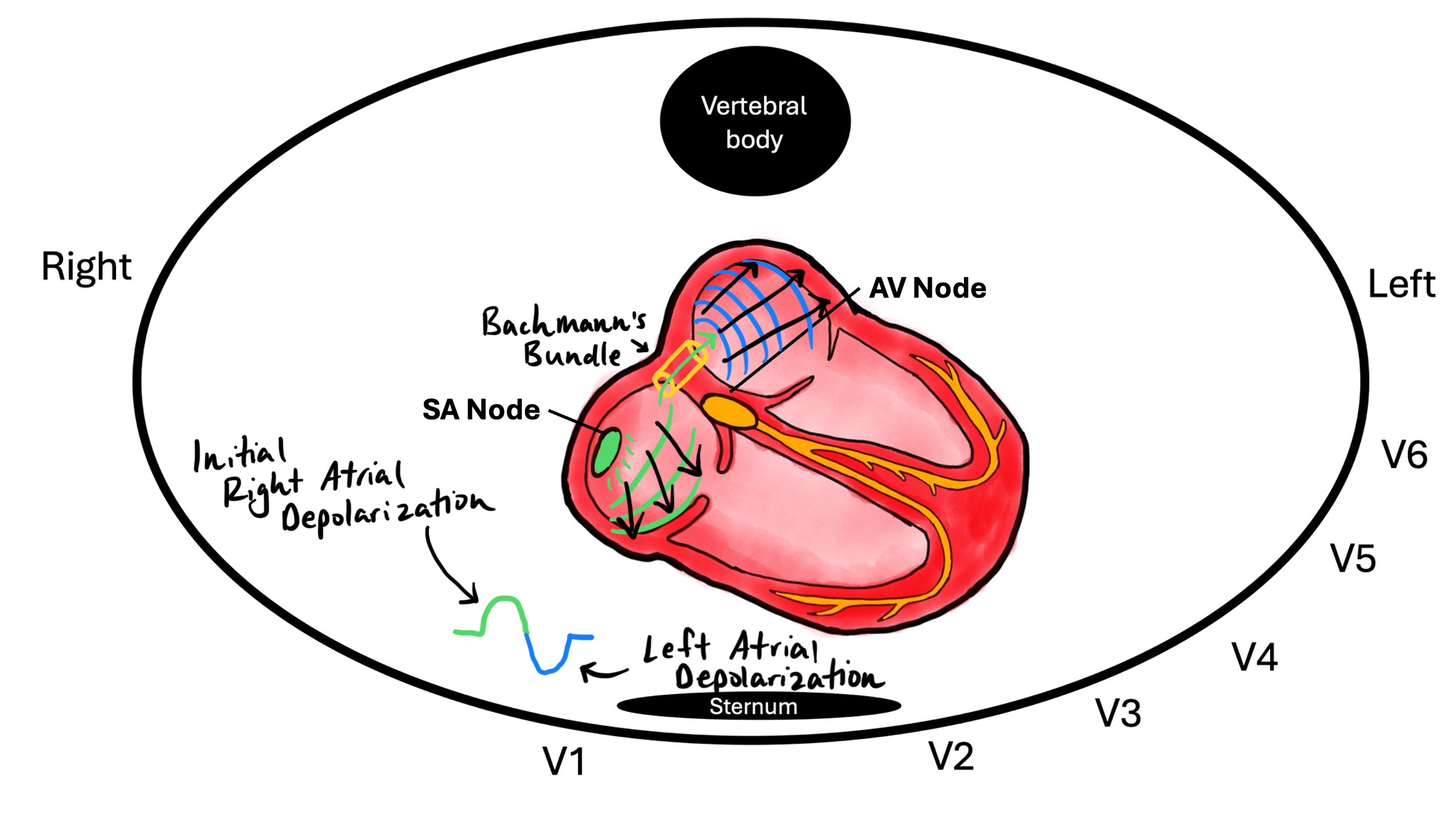
2. What Exactly Is Bachmann’s Bundle?
Bachmann’s bundle is a thick band of horizontally oriented atrial fibers running from the superior right atrium across the interatrial septum to the left atrial roof.
It is the primary—and fastest—interatrial conduction pathway.
Its role:
-
Ensures synchronous activation of both atria.
-
Delivers the sinus impulse to the LA early enough to preserve mechanical timing.
-
Establishes the predictable timing relationship between RA and LA components of the P wave.
If Bachmann’s bundle conducts normally:
-
RA and LA activation occur in a tight sequence.
-
Terminal P-wave negativity remains small and narrow.
If Bachmann’s bundle is delayed or diseased:
-
LA activation becomes late and more posterior.
-
The terminal P-wave vector becomes larger and more negative in V1.
This is precisely what PTFV1 measures.
3. How We Measure the P-Wave Terminal Force
PTFV1 =
Depth (mm) of the terminal negative P-wave portion in V1 × Duration (ms) of that negative component.
Why this works:
-
Increased LA mass → larger amplitude of the negative vector.
-
Delayed LA conduction (often via diseased Bachmann’s bundle) → prolonged duration of negativity.
-
A larger posterior/leftward vector → deeper and longer terminal negativity in V1.
Thus PTFV1 captures both structural enlargement and conduction delay, not just LA size.
4. When PTFV1 Becomes Abnormal: The Anatomical Basis
PTFV1 becomes more negative when:
A. Left atrial enlargement
-
More myocardium to depolarize.
-
Larger posterior-directed vector.
-
Produces deeper and broader terminal negativity.
B. Interatrial conduction delay
Often due to:
-
Fibrosis of Bachmann’s bundle
-
Atrial cardiomyopathy
-
Chronic pressure or volume overload
-
Inflammation or infiltrative disease
Delayed conduction prolongs the terminal P-wave portion, even if LA size is normal.
Enjoy ECG Lectures with Reid? Here is a special gift from Reid
100 High Yield Annotated ECGs
Click below to download this free resource.