Retrograde P Waves in Junctional Rhythms: Why They Appear Before, During, or After the QRS
Sep 17, 2025In sinus rhythm, atrial activation starts at the SA node and spreads downward, giving us upright P waves in the inferior leads (II, III, aVF) that precede every QRS. But in junctional rhythms or junctional ectopic beats, the origin of depolarization shifts to the atrioventricular (AV) junction. This anatomical change flips the conduction sequence: the ventricles and atria are activated from the middle outward.
The fascinating part? The retrograde P waves in junctional rhythms can show up before, during, or after the QRS complex. The exact timing depends on how fast the depolarization wavefronts reach the atria compared to the ventricles.
Anatomy Review: Where Junctional Beats Arise
-
AV Junction Location: The area just around the AV node and proximal His bundle.
-
Bidirectional Conduction: From here, impulses can travel antegrade (downward into the His-Purkinje system → ventricles) and retrograde (upward through the AV node into the atria).
-
Relative Timing: Whether the atria or ventricles depolarize first depends on which pathway is faster, and where the ectopic focus originates.
Physiology of Retrograde Atrial Activation
-
Retrograde conduction through the AV node is slower than Purkinje conduction downward.
-
This means the ventricles are usually activated first, unless the retrograde pathway is particularly brisk.
-
The relative speed determines where the retrograde P wave lands on the ECG.
The Three Possible Locations of Retrograde P Waves
1. Before the QRS Complex (Short PR)
-
Mechanism: Retrograde conduction to the atria occurs slightly faster than antegrade conduction to the ventricles.
-
ECG Appearance:
-
Inverted P wave appears just before the QRS.
-
The PR interval is short (<120 ms).
-

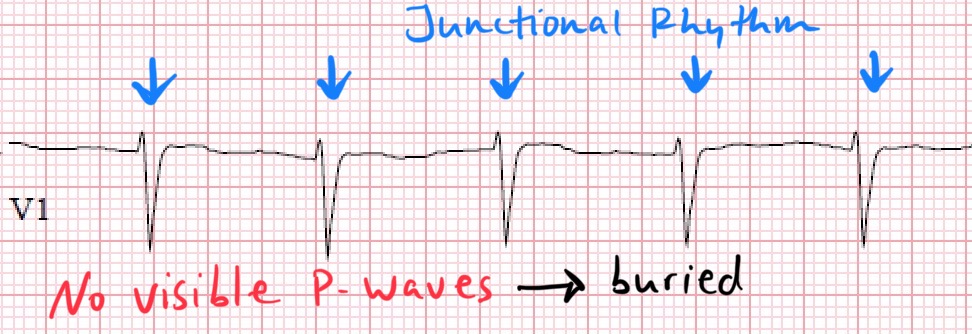
2. During the QRS Complex (Hidden P)
-
Mechanism: Retrograde atrial activation and ventricular activation happen nearly simultaneously.
-
ECG Appearance:
-
No visible P wave because it is buried inside the QRS complex.
-
The QRS looks narrow and normal, but no preceding P is seen.
-
3. After the QRS Complex (Retrograde P Following)
-
Mechanism: Antegrade conduction to the ventricles is faster than retrograde conduction to the atria.
-
ECG Appearance:
-
Narrow QRS occurs first.
-
Inverted P wave appears in the ST segment or early T wave.
-
The RP interval varies but is usually short (<200 ms).
-

Key ECG Lead to Look At
-
Inferior leads (II, III, aVF): Retrograde atrial activation moves upward (superiorly) in the chest, which is away from the inferior leads → inverted P waves here are the most reliable marker of retrograde conduction.
Clinical Relevance
-
Escape vs. Ectopic:
-
Junctional escape beats are a protective mechanism when the SA node fails.
-
Junctional ectopic beats are premature and may occur with digitalis toxicity, enhanced automaticity, or reentry.
-
-
Differentiation: Recognizing the location of retrograde P waves helps distinguish junctional rhythms from other supraventricular arrhythmias.
-
AV Dissociation: If retrograde conduction is absent, the atria and ventricles depolarize independently → no retrograde P waves will be seen.
Enjoy ECG Lectures with Reid? Here is a special gift from Reid
100 High Yield Annotated ECGs
Click below to download this free resource.