1:1 Atrial Flutter — When the AV Node Stops Protecting the Ventricles
Nov 10, 2025Atrial flutter is typically a well-behaved arrhythmia — a rapid, organized atrial rhythm whose ventricular response is tempered by the AV node’s intrinsic filtering. But occasionally, this safety mechanism fails, allowing 1:1 conductionfrom atria to ventricles.
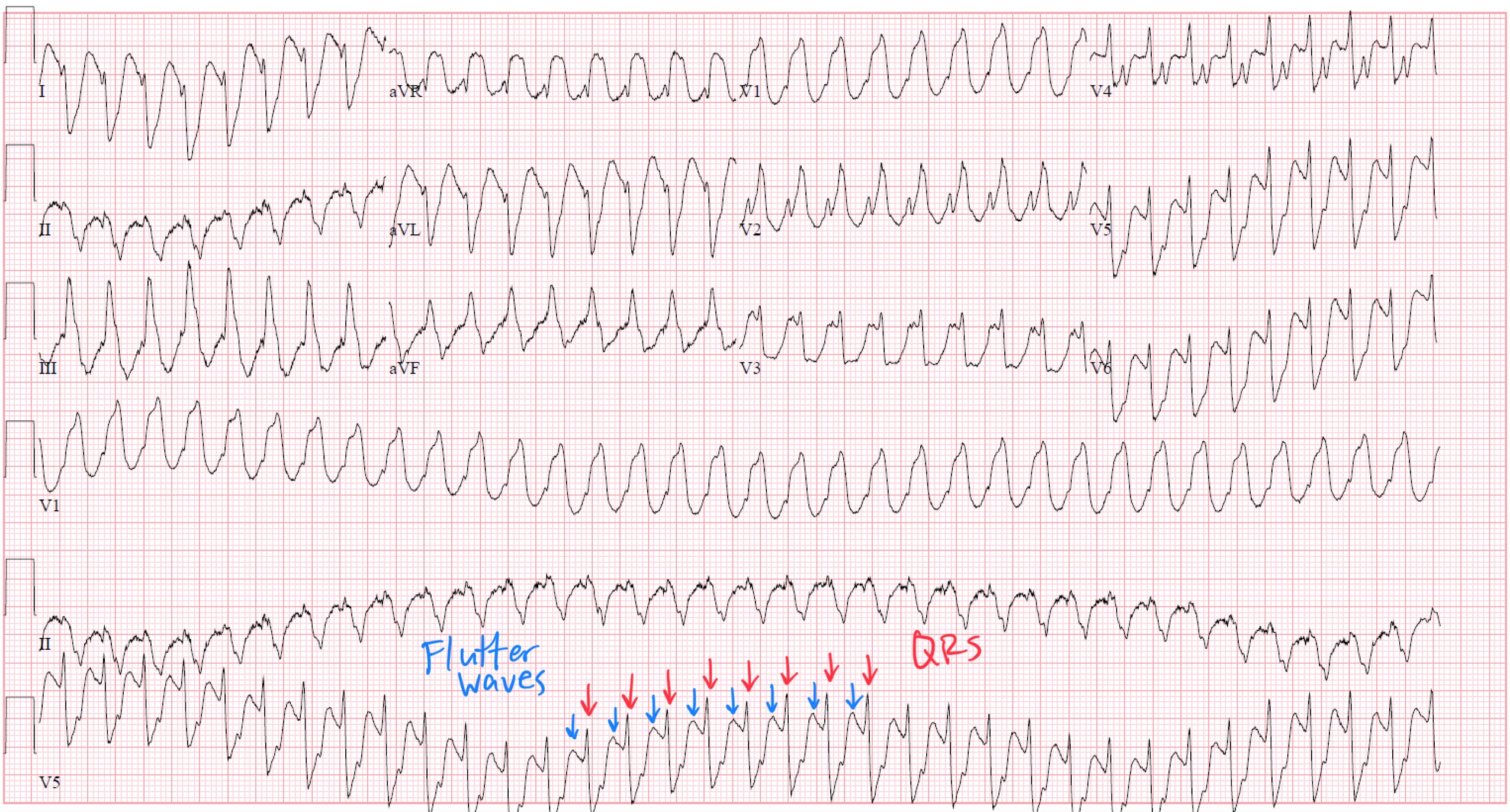
The result? Ventricular rates exceeding 250 bpm, often misdiagnosed as ventricular tachycardia, and a clinical situation that can rapidly become unstable.
The Anatomy and Electrophysiology of Atrial Flutter
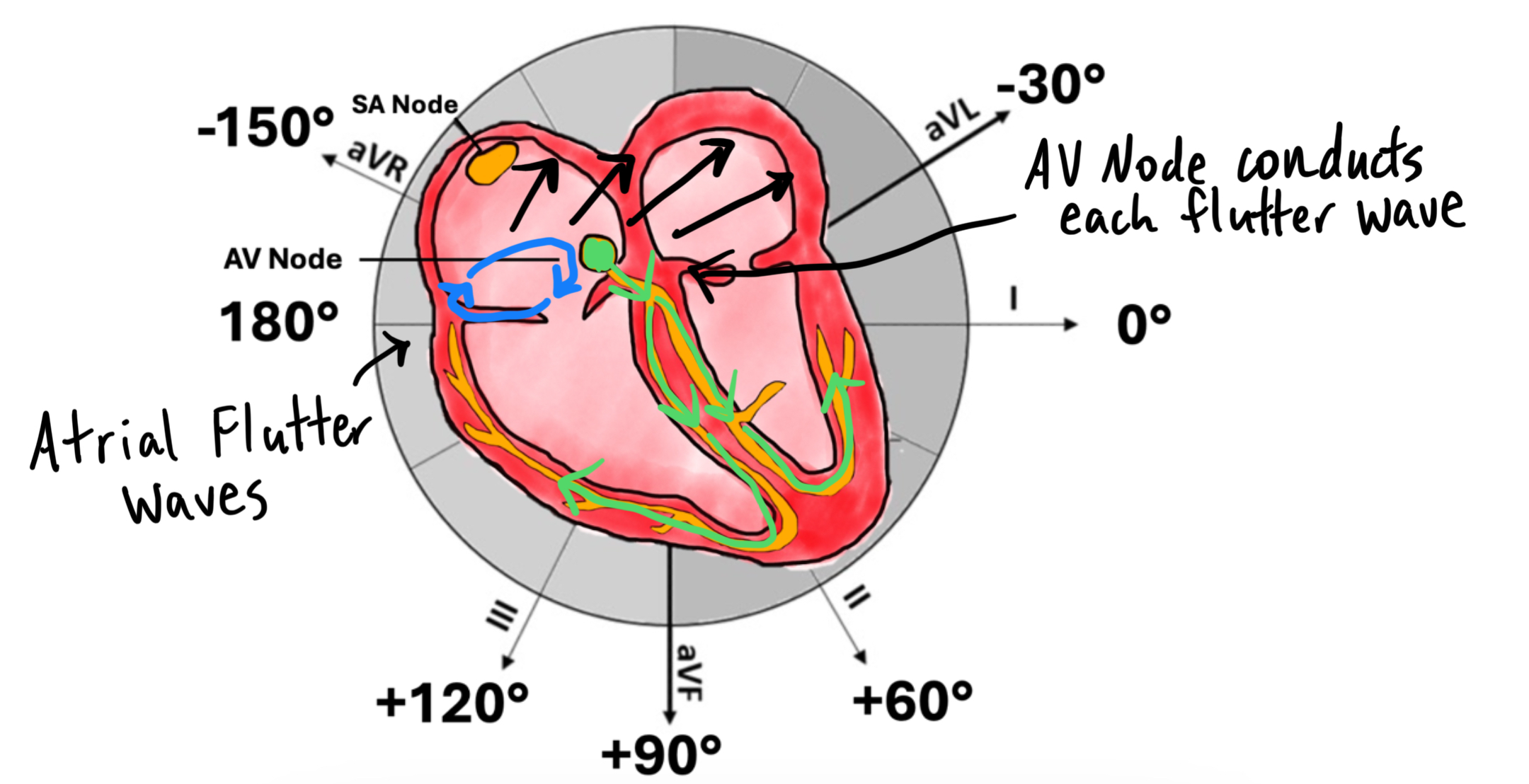
Atrial flutter is produced by a macroreentrant circuit, most commonly counterclockwise around the tricuspid annulus(typical flutter).
-
Atrial rate: ~240–350 bpm
-
Circuit location: Right atrium, using the cavotricuspid isthmus as the slow conduction zone
-
P waves: Flutter waves (“sawtooth”) in inferior leads (II, III, aVF), typically negative in these leads and positive in V1
The AV node normally exhibits decremental conduction, meaning that as atrial rates increase, conduction velocity slows, limiting how many impulses reach the ventricles.
This protects the ventricles from excessive rates — usually allowing 2:1, 3:1, or 4:1 conduction ratios.
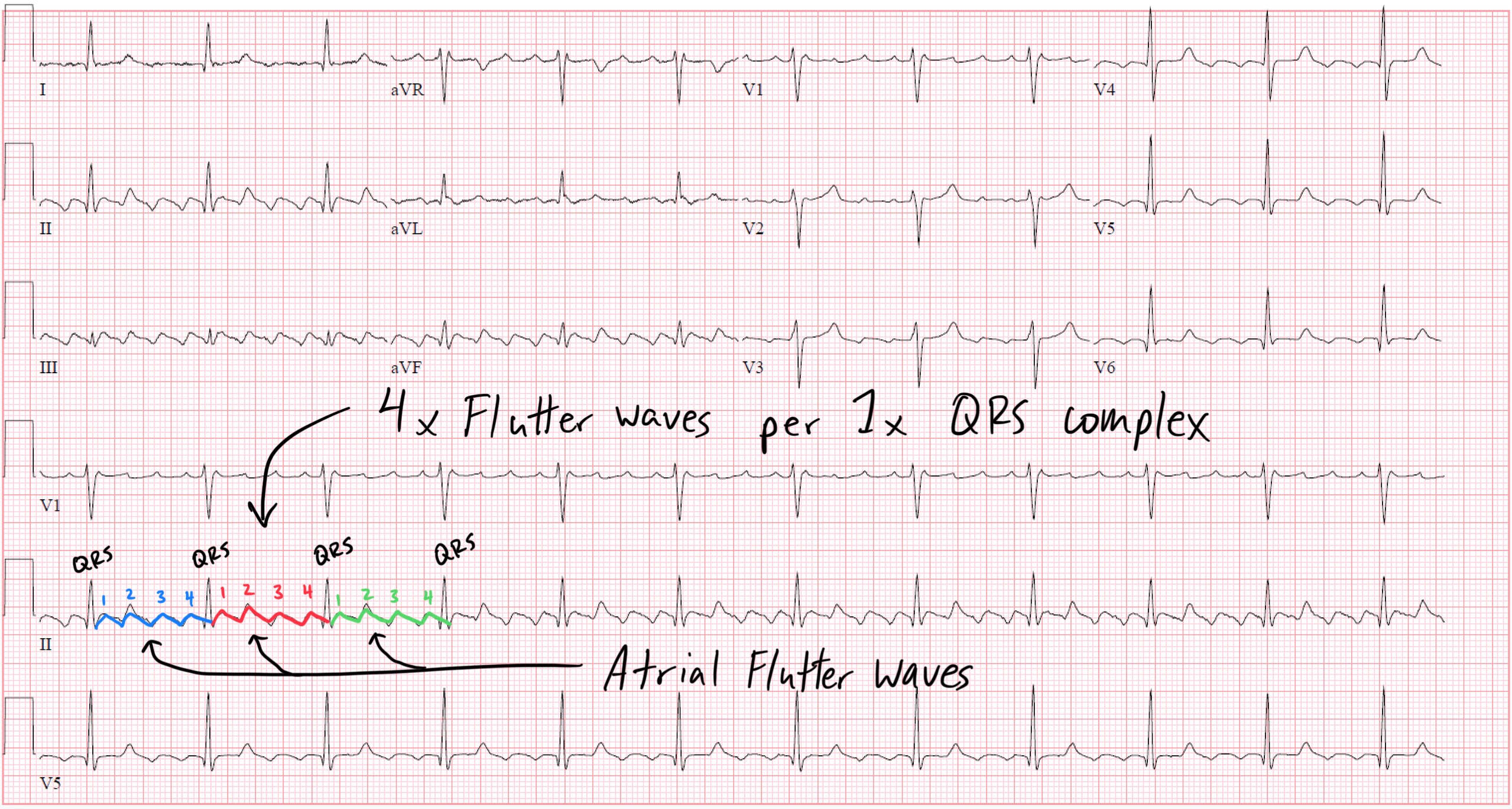
Example: Atrial Flutter with 4:1 AV Conduction
When the AV Node Fails: 1:1 Conduction
In 1:1 atrial flutter, every atrial depolarization conducts through to the ventricles. This requires:
-
A very short AV nodal refractory period, and
-
Enhanced sympathetic tone or drug effect that increases AV nodal conduction velocity.
The ventricular rate now mirrors the atrial rate — often 240–300 bpm, a range at which hemodynamic collapse is common.
Common Causes of 1:1 Atrial Flutter
1. Catecholamine Excess
-
Mechanism: Increased sympathetic tone shortens AV nodal refractoriness.
-
Clinical settings: Exercise, stress, sepsis, hyperthyroidism, or stimulant use (cocaine, amphetamines).
2. Class IC Antiarrhythmics (Flecainide, Propafenone)
-
Mechanism: These slow intra-atrial conduction without prolonging AV nodal refractoriness.
-
This allows the flutter circuit to slow (often 200–250 bpm) — now within the AV node’s conduction capability — promoting 1:1 AV conduction.
-
Clinical pearl: Always co-administer an AV nodal blocker (beta-blocker or calcium channel blocker) when using class IC drugs in atrial arrhythmias.
3. Digoxin Toxicity
-
Usually enhances vagal tone and slows AV conduction, but paradoxically may cause ectopic junctional rhythms that make diagnosis confusing.
-
Rarely, increased automaticity or arrhythmogenic effects of toxicity may mimic rapid conduction patterns.
4. Accessory Pathways (Pre-excitation)
-
In Wolff–Parkinson–White (WPW), impulses can bypass the AV node entirely and conduct 1:1 via the accessory pathway, mimicking 1:1 flutter or SVT with aberrancy.
ECG Findings
Key ECG clue:
If a “regular wide-complex tachycardia” has a ventricular rate near 250 bpm in a patient on flecainide, suspect 1:1 atrial flutter.
Look carefully in V1 or inferior leads — you may find subtle flutter waves embedded within the T waves or ST segment.
Mechanistic Insight: The Role of the AV Node
Under normal physiology, the AV node acts as a gatekeeper, filtering high-frequency atrial impulses through decremental conduction — a property determined by calcium-dependent slow-channel depolarization.
-
Sympathetic stimulation (β-adrenergic activity) enhances calcium current, shortening AV nodal refractoriness→ more impulses conduct.
-
Parasympathetic stimulation (acetylcholine) reduces calcium influx, prolonging AV nodal refractoriness → fewer impulses conduct.
In 1:1 flutter, the balance shifts toward sympathetic predominance or pharmacologic enhancement of AV nodal conduction, allowing full transmission of the atrial circuit’s rapid rhythm.
Clinical Implications
1. Misdiagnosis as Ventricular Tachycardia
At rates of 250 bpm, 1:1 flutter can appear as a regular wide-complex tachycardia due to aberrant conduction.
If uncertain, always treat as VT until proven otherwise — misdiagnosis can be fatal, especially if verapamil or adenosine is administered in pre-excited arrhythmias.
2. Hemodynamic Collapse
Ventricular rates above 220–240 bpm reduce filling time dramatically, leading to hypotension, syncope, or cardiac arrest.
3. Treatment
-
Immediate rate control: IV beta-blocker or non-dihydropyridine calcium channel blocker (verapamil, diltiazem).
-
Unstable patients: Electrical cardioversion.
-
Long-term: Ablation of the cavotricuspid isthmus is curative in >90% of typical flutter.
-
If on Class IC drugs: Stop the agent and ensure AV nodal blockade before re-initiation.
Take-Home Points
-
Atrial flutter usually conducts with a 2:1 or higher AV block due to decremental AV nodal physiology.
-
1:1 flutter occurs when AV nodal refractoriness shortens — from sympathetic stimulation or Class IC drug use.
-
The ventricular rate often exceeds 240 bpm, producing a regular, potentially wide tachycardia that mimics VT.
-
On ECG, flutter waves may be subtle or buried — look in V1 or inferior leads for sawtooth activity.
-
Always co-administer AV nodal blockers with Class IC antiarrhythmics to prevent 1:1 conduction.
Enjoy ECG Lectures with Reid? Here is a special gift from Reid
100 High Yield Annotated ECGs
Click below to download this free resource.